1. Bozkurt B, Coats AJS, Tsutsui H, et al. Universal definition and classification of heart failure:a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure:Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur J Heart Fail 23(3):352-380, 2021.
2. Bozkurt B, Coats AJ, Tsutsui H, et al. Universal Definition and Classification of Heart Failure:A Report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J Card Fail, 2021.
3. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure:The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129-2200, 2016.
4. McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42(36):3599-3726, 2021.
5. Schrier RW. Water and sodium retention in edematous disorders:role of vasopressin and aldosterone. Am J Med 119(7 Suppl 1):S47-53, 2006.
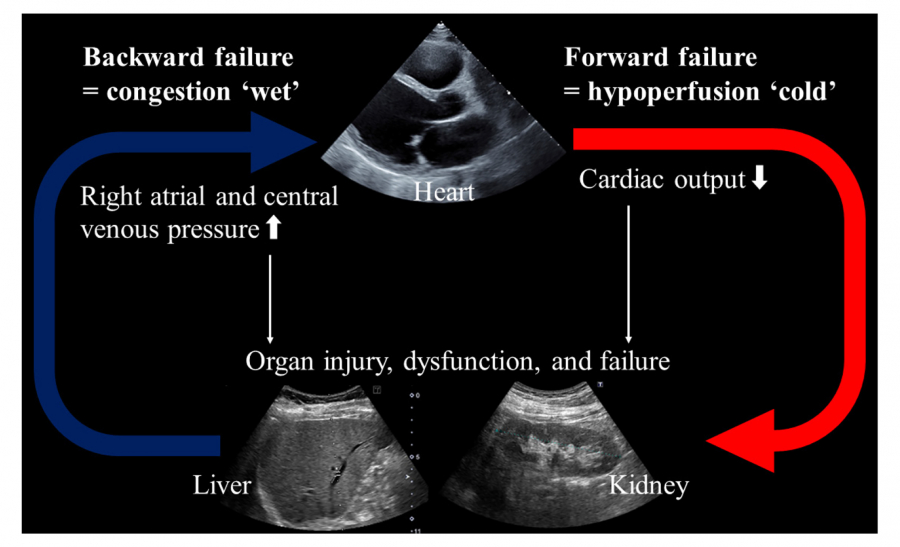
6. Harjola VP, Mullens W, Banaszewski M, et al. Organ dysfunction, injury and failure in acute heart failure:from pathophysiology to diagnosis and management. A review on behalf of the Acute Heart Failure Committee of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail 19(7):821-836, 2017.
7. Yoshihisa A, Takeishi Y. Heart failure and sleep disordered breathing. Fukushima J Med Sci 63(2):32-38, 2017.
8. Xanthopoulos A, Starling RC, Kitai T, Triposkiadis F. Heart Failure and Liver Disease:Cardiohepatic Interactions. JACC Heart Fail 7(2):87-97, 2019.
9. Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol 52(19):1527-1539, 2008.
10. Yoshihisa A, Kanno Y, Ichijo Y, et al. Incidence and subsequent prognostic impacts of gastrointestinal bleeding in patients with heart failure. Eur J Prev Cardiol 27(6):664-666, 2020.
11. Moller S, Bernardi M. Interactions of the heart and the liver. Eur Heart J 34(36):2804-2811, 2013.
12. Samsky MD, Patel CB, DeWald TA, et al. Cardiohepatic interactions in heart failure:an overview and clinical implications. J Am Coll Cardiol 61(24):2397-2405, 2013.
13. Nikolaou M, Parissis J, Yilmaz MB, et al. Liver function abnormalities, clinical profile, and outcome in acute decompensated heart failure. Eur Heart J 34(10):742-749, 2013.
14. Birrer R, Takuda Y, Takara T. Hypoxic hepatopathy:pathophysiology and prognosis. Intern Med 46(14):1063-1070, 2007.
15. Jalal Z, Iriart X, De Ledinghen V, et al. Liver stiffness measurements for evaluation of central venous pressure in congenital heart diseases. Heart 101(18):1499-1504, 2015.
16. Taniguchi T, Sakata Y, Ohtani T, et al. Usefulness of transient elastography for noninvasive and reliable estimation of right-sided filling pressure in heart failure. Am J Cardiol 113(3):552-558, 2014.
17. Sato Y, Yoshihisa A, Kanno Y, et al. Liver stiffness assessed by Fibrosis-4 index predicts mortality in patients with heart failure. Open Heart 4(1):e000598, 2017.
18. Yoshihisa A, Ishibashi S, Matsuda M, et al. Clinical Implications of Hepatic Hemodynamic Evaluation by Abdominal Ultrasonographic Imaging in Patients With Heart Failure. J Am Heart Assoc 9(15):e016689, 2020.
19. Nohria A, Tsang SW, Fang JC, et al. Clinical assessment identifies hemodynamic profiles that predict outcomes in patients admitted with heart failure. J Am Coll Cardiol 41(10):1797-1804, 2003.
20. Ohara H, Yoshihisa A, Ishibashi S, et al. Hepatic Venous Stasis Index Reflects Hepatic Congestion and Predicts Adverse Outcomes in Patients With Heart Failure. J Am Heart Assoc 12(12):e029857, 2023.
21. Misaka T, Yoshihisa A, Ichijo Y, et al. Prognostic significance of spleen shear wave elastography and dispersion in patients with heart failure:the crucial role of cardio-splenic axis. Clin Res Cardiol 112(7):942-953, 2023.
22. Tomita Y, Misaka T, Yoshihisa A, et al. Decreases in hepatokine Fetuin-A levels are associated with hepatic hypoperfusion and predict cardiac outcomes in patients with heart failure. Clin Res Cardiol 111(10):1104-1112, 2022.
23. Sugawara Y, Yoshihisa A, Ishibashi S, et al. Liver Congestion Assessed by Hepatic Vein Waveforms in Patients With Heart Failure. CJC Open 3(6):778-786, 2021.
24. Ronco C, McCullough P, Anker SD, et al. Cardio-renal syndromes:report from the consensus conference of the acute dialysis quality initiative. Eur Heart J 31(6):703-711, 2010.
25. Nagai T, Yoshikawa T, Saito Y, et al. Clinical Characteristics, Management, and Outcomes of Japanese Patients Hospitalized for Heart Failure With Preserved Ejection Fraction - A Report From the Japanese Heart Failure Syndrome With Preserved Ejection Fraction (JASPER) Registry. Circ J 82(6):1534-1545, 2018.
26. Sato Y, Yoshihisa A, Oikawa M, et al. Prognostic Impact of Worsening Renal Function in Hospitalized Heart Failure Patients With Preserved Ejection Fraction:A Report From the JASPER Registry. J Card Fail 25(8):631-642, 2019.
27. Yoshihisa A, Watanabe K, Sato Y, et al. Intrarenal Doppler ultrasonography reflects hemodynamics and predicts prognosis in patients with heart failure. Sci Rep 10(1):22257, 2020.
28. Ohara H, Yoshihisa A, Horikoshi Y, et al. Renal Venous Stasis Index Reflects Renal Congestion and Predicts Adverse Outcomes in Patients With Heart Failure. Front Cardiovasc Med 9:772466, 2022.
29. Klein I, Danzi S. Thyroid disease and the heart. Circulation 116(15):1725-1735, 2007.
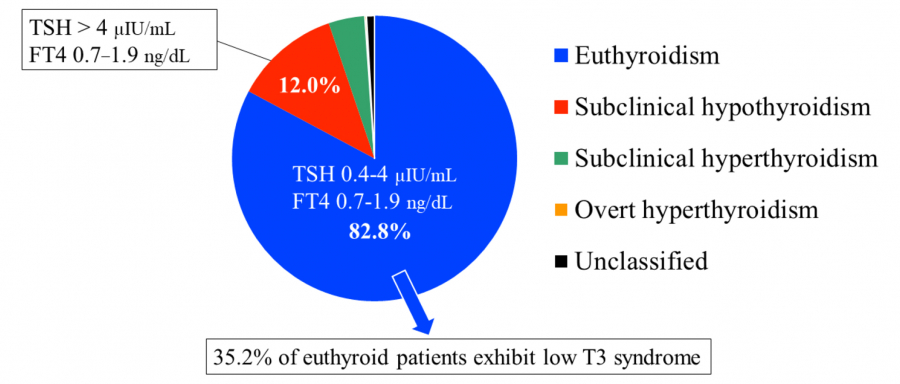
30. Sato Y, Yoshihisa A, Kimishima Y, et al. Subclinical Hypothyroidism Is Associated With Adverse Prognosis in Heart Failure Patients. Can J Cardiol 34(1):80-87, 2018.
31. Pearce SH, Brabant G, Duntas LH, et al. 2013 ETA Guideline:Management of Subclinical Hypothyroidism. Eur Thyroid J 2(4):215-228, 2013.
32. Utiger RD. Altered thyroid function in nonthyroidal illness and surgery. To treat or not to treat? N Engl J Med 333(23):1562-1563, 1995.
33. Hamilton MA, Stevenson LW, Luu M, Walden JA. Altered thyroid hormone metabolism in advanced heart failure. J Am Coll Cardiol 16(1):91-95, 1990.
34. Sato Y, Yoshihisa A, Kimishima Y, et al. Low T3 Syndrome Is Associated With High Mortality in Hospitalized Patients With Heart Failure. J Card Fail 25(3):195-203, 2019.
35. Parent S, Cujec B. Subclinical Hypothyroidism and Heart Failure:Chicken or Egg? Can J Cardiol 34(1):11-12, 2018.
36. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure:A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 145(18):e895-e1032, 2022.
37. Tsutsui H, Isobe M, Ito H, et al. JCS 2017/JHFS 2017 Guideline on Diagnosis and Treatment of Acute and Chronic Heart Failure- Digest Version. Circ J 83(10):2084-2184, 2019.
38. Laugsand LE, Strand LB, Platou C, Vatten LJ, Janszky I. Insomnia and the risk of incident heart failure:a population study. Eur Heart J 35(21):1382-1393, 2014.
39. Kanno Y, Yoshihisa A, Watanabe S, et al. Prognostic Significance of Insomnia in Heart Failure. Circ J 80(7):1571-1577, 2016.
40. Morin CM, Benca R. Chronic insomnia. Lancet 379(9821):1129-1141, 2012.
41. Buysse DJ, Angst J, Gamma A, Ajdacic V, Eich D, Rossler W. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep 31(4):473-480, 2008.
42. Dew MA, Hoch CC, Buysse DJ, et al. Healthy older adults’ sleep predicts all-cause mortality at 4 to 19 years of follow-up. Psychosom Med 65(1):63-73, 2003.
43. Sato Y, Yoshihisa A, Hotsuki Y, et al. Associations of Benzodiazepine With Adverse Prognosis in Heart Failure Patients With Insomnia. J Am Heart Assoc 9(7):e013982, 2020.
44. Tannenbaum C, Martin P, Tamblyn R, Benedetti A, Ahmed S. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education:the EMPOWER cluster randomized trial. JAMA Intern Med 174(6):890-898, 2014.
45. Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD, Clinical Guidelines Committee of the American College of P. Management of Chronic Insomnia Disorder in Adults:A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med 165(2):125-133, 2016.
46. Evans WJ, Morley JE, Argiles J, et al. Cachexia:a new definition. Clin Nutr 27(6):793-799, 2008.
47. von Haehling S, Anker SD. Cachexia as a major underestimated and unmet medical need:facts and numbers. J Cachexia Sarcopenia Muscle 1(1):1-5, 2010.
48. von Haehling S, Lainscak M, Springer J, Anker SD. Cardiac cachexia:a systematic overview. Pharmacol Ther 121(3):227-252, 2009.
49. Loncar G, Springer J, Anker M, Doehner W, Lainscak M. Cardiac cachexia:hic et nunc. J Cachexia Sarcopenia Muscle 7(3):246-260, 2016.
50. Sato Y, Yoshihisa A, Kimishima Y, et al. Prognostic factors in heart failure patients with cardiac cachexia. J Geriatr Cardiol 17(1):26-34, 2020.
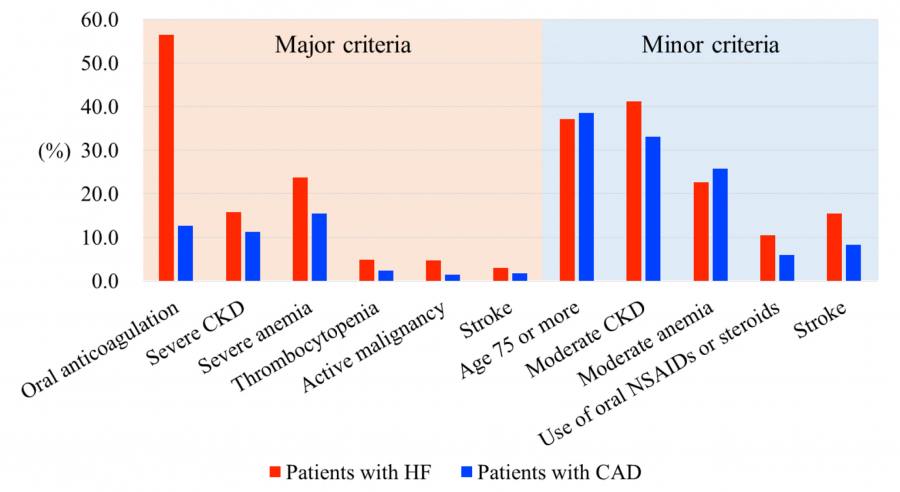
51. Urban P, Mehran R, Colleran R, et al. Defining high bleeding risk in patients undergoing percutaneous coronary intervention:a consensus document from the Academic Research Consortium for High Bleeding Risk. Eur Heart J 40(31):2632-2653, 2019.
52. Urban P, Mehran R, Colleran R, et al. Defining High Bleeding Risk in Patients Undergoing Percutaneous Coronary Intervention. Circulation 140(3):240-261, 2019.
53. Miura K, Shimada T, Ohya M, et al. Prevalence of the Academic Research Consortium for High Bleeding Risk Criteria and Prognostic Value of a Simplified Definition. Circ J 84(9):1560-1567, 2020.
54. Sato Y, Yoshihisa A, Takeishi R, et al. Simplified Academic Research Consortium for High Bleeding Risk (ARC-HBR) Definition Predicts Bleeding Events in Patients With Heart Failure. Circ J 86(1):147-155, 2021.
55. Fujii T, Ikari Y. Predictive Ability of Academic Research Consortium for High Bleeding Risk Criteria in ST-Elevation Myocardial Infarction Patients Undergoing Primary Coronary Intervention. Circ J 85(2):159-165, 2021.
56. Nakamura M, Kadota K, Nakao K, et al. High bleeding risk and clinical outcomes in East Asian patients undergoing percutaneous coronary intervention:the PENDULUM registry. EuroIntervention 16(14):1154-1162, 2021.
57. Nochioka K. Simplifying Bleeding Risk Assessment in Heart Failure. Circ J 86(1):156-157, 2021.
58. Yoshihisa A, Sato Y, Sato T, Suzuki S, Oikawa M, Takeishi Y. Better clinical outcome with direct oral anticoagulants in hospitalized heart failure patients with atrial fibrillation. BMC Cardiovasc Disord 18(1):11, 2018.
59. Nakamura M, Kimura K, Kimura T, et al. JCS 2020 Guideline Focused Update on Antithrombotic Therapy in Patients With Coronary Artery Disease. Circ J 84(5):831-865, 2020.