Background:Laparoscopic and endoscopic cooperative surgery (LECS) is a well-recognized surgical procedure for gastric gastrointestinal stromal tumor (GIST). In this report, we describe the clinical outcomes of LECS procedures for gastric GIST in our institution.
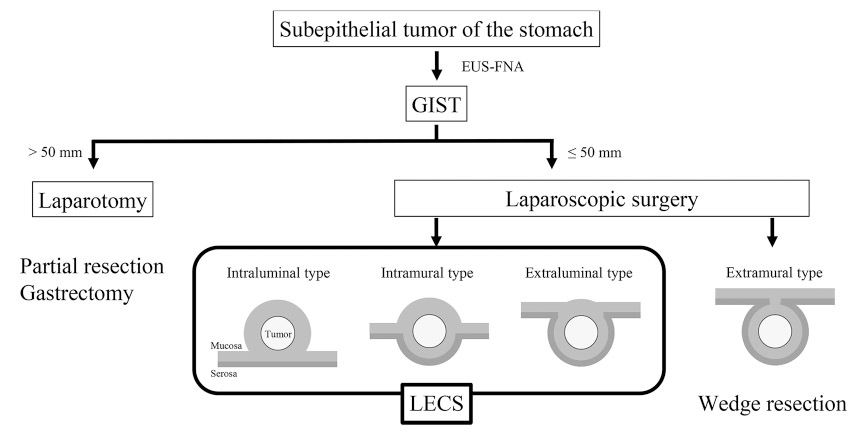
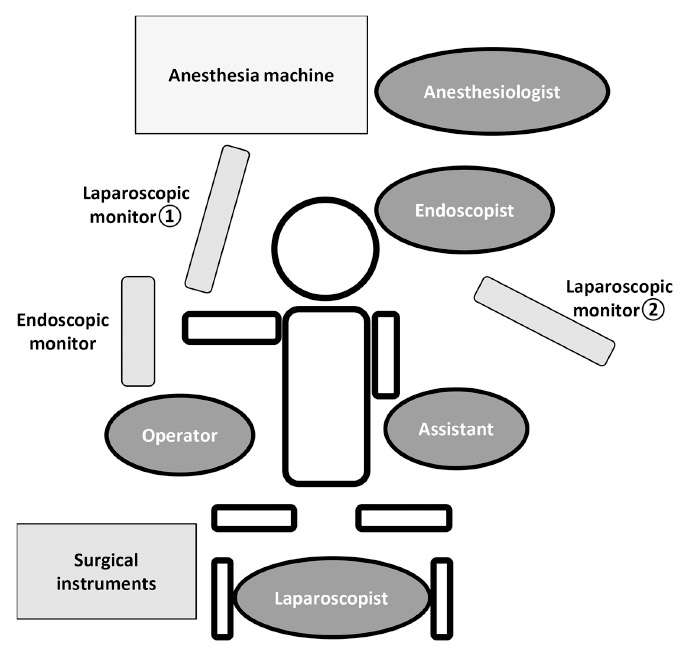
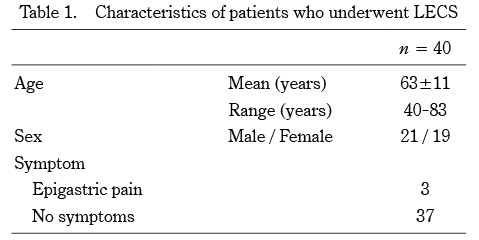
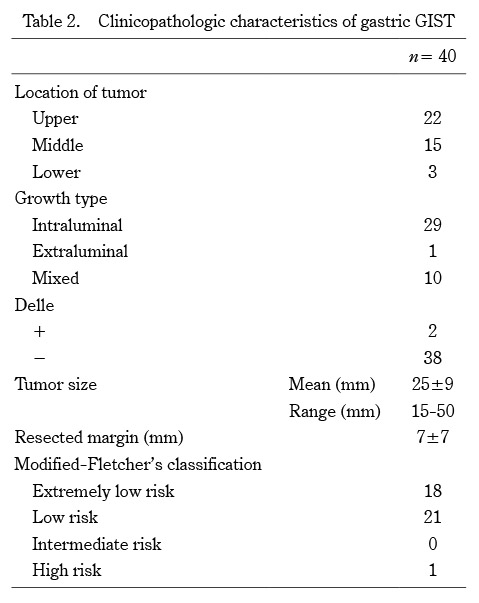
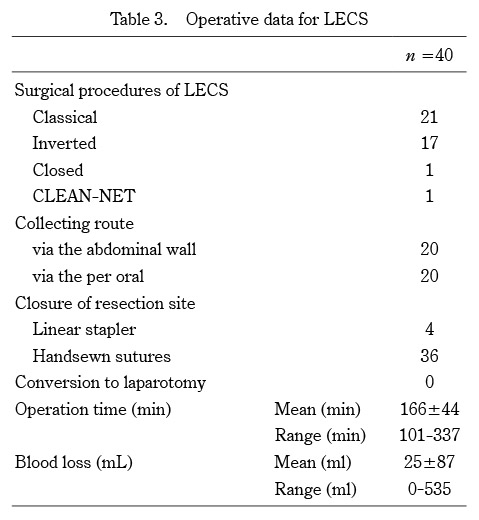
Methods:We performed LECS procedures, including classical LECS, inverted LECS, closed LECS, and combination of laparoscopic and endoscopic approaches to neoplasia with non-exposure technique (CLEAN-NET), in 40 gastric intraluminal and intramural type GIST patients, whose tumors were ≤ 50 mm in diameter, between September 2012 and December 2020. The patient background, surgical outcomes, postoperative morbidity and mortality, as well as the tumors’ clinicopathological characteristics were analyzed retrospectively.
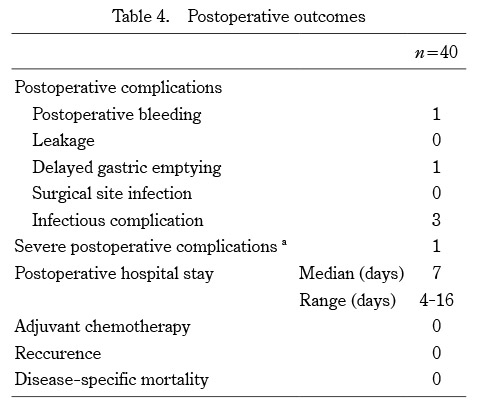
Results:Pathological findings showed that most patients had a low or very low risk of tumor recurrence, while one patient had a high risk according to the modified-Fletcher’s classification. The median length of postoperative hospital stay was 7 days. Only one patient had severe postoperative grade III complications according to the Clavien-Dindo (C-D) classification, after closed LECS, but was treated successfully with endoscopic hemostasis for postoperative hemorrhage. The remaining patients treated with LECS did not have severe complications. During the follow-up period (median, 31 months), all patients were disease-free, with no tumor recurrence or metastases.
Conclusion:LECS is a safe surgical procedure for gastric intraluminal and intramural type GIST ≤ 50 mm in diameter, with good clinical outcomes.